A new NHS trial is using a home monitoring app combined with artificial intelligence (AI) to predict when people living with chronic lung conditions like cystic fibrosis may be developing a severe infection and reduce the chance of them ending up in hospital.
ACE-CF uses an app that takes measurements added by an individual such as lung function and blood oxygen levels, and uses an algorithm to determine if their health is deteriorating and an infection may be developing.
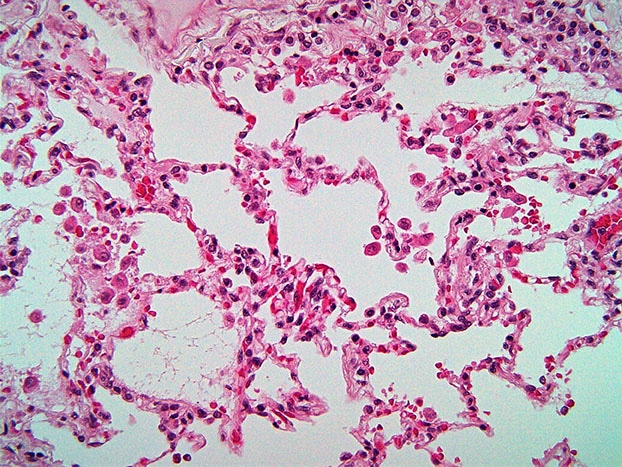
People living with chronic lung conditions like cystic fibrosis and bronchiectasis frequently experience exacerbations – a worsening of symptoms that can further damage their lungs – which often involves chest infections. These can be serious and require admission to hospital for treatment with antibiotics. These stays can last weeks or months, severely disrupting everyday life and cause further damage to the lungs.
The app is designed to work as an ‘early warning system’ and let people living with these conditions know if an infection could be developing up to 10 days earlier. They can then contact their healthcare professional to seek advice and, if needed, receive treatment before symptoms begin, to reduce the chances of ending up in hospital and prevent further damage to their lungs.
The use of artificial intelligence in home monitoring came as part of a collaboration between a team of researchers led by Professor Andres Floto, a Research Director of the Cambridge Centre for Lung Infection at Royal Papworth Hospital NHS Foundation Trust, and Microsoft Research. They used data collected from previous projects to show that AI can be used to predict if a patient’s health may deteriorate.
“Our previous research looked at how artificial intelligence could be used to detect when a person with cystic fibrosis had a decline in their health and could be at risk of developing a lung infection.
“We are delighted to be able to continue our innovative work using AI to detect lung infections much earlier than standard care and improve the quality of life of people living with these challenging lung conditions. This approach could be used for other health conditions as well in future.”
Turning this research into something that could be trialled was led by Kirsty Hill, a project manager and her husband, David, a software engineer at Microsoft, who were inspired to help their son, George, who was born with cystic fibrosis, a genetic condition.
“George was diagnosed with cystic fibrosis when he was one; he was very ill and ended up spending lots of time in hospital receiving antibiotics for severe infections. We wanted to use our expertise to make a difference for George and others living with cystic fibrosis and develop a way to help monitor key data to empower them to better understand and self-manage their condition.”
The family founded a company, Magic Bullet, and joined forces with Royal Papworth Hospital to test the AI in another trial called Project Breathe. They have now teamed up with LifeArc and the NIHR to use the system in the ACE-CF trial to test the machine learning in real-time with patients.
“Our hope now is to use machine learning to not only keep well people out of hospital, but also get unwell people seen sooner and, if needed, start treatments sooner, so that they can confidently go about their lives and worry less about the uncertainty of living with cystic fibrosis,” Kirsty added.
This trial is based at Royal Papworth Hospital, which is the UK’s leading heart, lung and sleep hospital, and involves 10 centres across the UK with the aim of recruiting 400 patients.
Fifty are already enrolled at Royal Papworth, including Sammie Read, 43, from Suffolk, who lives with cystic fibrosis and has seen first-hand the impact home monitoring has had on her life since being on an earlier version of the trial.
“My life is not as consumed by cystic fibrosis as it was before. I used to regularly be an inpatient at Royal Papworth every 3 to 4 months for up to 2 weeks at a time and was on up to 40 pills a day.
“I also used to have an outpatient appointment every 6 weeks, which would involve a one-hour drive to Cambridge and back. Thanks to home monitoring these are now every 4 months instead.”
“I sleep better because I haven’t got the stress and worry about my health 24/7. I’ve also returned to work part-time as an accountant for a garage, which isn’t something I was previously able to do because of all the appointments. Now I can set a life-long goal.
“Previously I thought I’d be lucky to see my son finish school at 18. I remember crying when he finished primary school. Now he’s 23 and if he ever gets married and has children, I’d like to think I’ll be there.”
The trial is now being expanded to include patients living with bronchiectasis, another chronic condition, where the airways of the lungs have become widened leading to a build-up of excess mucus that can make the lungs more vulnerable to infection.
The Bronch-Ex study is being funded by LifeArc as part of our wider £100m investment in improving outcomes for people living with chronic respiratory infections by 2030, and the NIHR.
Steven Tait, Project Lead at LifeArc, said “The ACE-CF and Bronch-Ex trials are prime examples of LifeArc’s ambition to help deliver more effective care for people living with conditions like cystic fibrosis and bronchiectasis. The system we’re trialling can help with earlier detection of flare-ups, which will enable earlier interventions to avoid unnecessary trips to the hospital, and empower patients by allowing them to self-monitor their condition. It could also be used to help people living with other chronic lung conditions like Chronic Obstructive Pulmonary Disease (COPD) and even asthma in future.”
This empowerment is something Kirsty hopes more people living with chronic lung conditions can feel and not have their lives controlled by their condition, “George hasn’t had any exacerbations recently and is now training for his dream job, to become a rollercoaster engineer. He’s thriving and I want this for everyone living with CF and other chronic lung conditions.”
Patients living with bronchiectasis are encouraged to find out more and see if they are eligible for the Bronch-EX study by going to the trial website.
Professor Mike Lewis, NIHR’s Scientific Director for Innovation, said:”The NIHR is proud to be supporting a suite of AI research projects like this one, all aiming to use cutting-edge technology to help improve treatment and quality of life for people with significant health conditions. Identifying lung infections early in people with CF and bronchiectasis could help reduce long-term lung damage, as well as cutting the number of hospital appointments that they need to attend – the potential to improve their quality of life is really exciting.”
Dr Lucy Allen, Director of Research and Healthcare Data at Cystic Fibrosis Trust said, “We’re delighted that Cystic Fibrosis Trust support for the earlier SMARTCARE research study and for the CF Innovation Hub on lung health at the University of Cambridge has led to the development of the ACE-CF trial. Predicting flare ups in lung health will make a significant difference for people with CF and their families, keeping their lungs healthier for longer and reducing the disruption to day-to-day life caused by lengthy hospital stays and aggressive treatments. It’s fantastic that this approach may also help people living with other lung conditions too”.
Media contact
Hannah Severyn
Head of Media and PR at LifeArc