MND Drug Repurposing Programme: Enhancing the MND ecosystem’s approach to drug repurposing
We’re funding high-quality preclinical studies and building a collaborative network to improve drug repurposing and trial readiness in motor neuron disease (MND).

Overview
Drug repurposing can offer a faster route to the clinic than traditional drug discovery, as medicines that are already approved for other conditions have established safety profiles. However, when repurposing candidates enter clinical trials without a detailed understanding of how the drug works in the new indication, trials are more likely to fail, and time, efforts and resources are wasted.
This programme funds and supports global research to address the challenges of drug repurposing in MND. Projects will generate robust preclinical evidence for drug candidates, to increase confidence in their selection for clinical trials, while ensuring that ineffective candidates ‘fail fast’ – avoiding unnecessary progression.
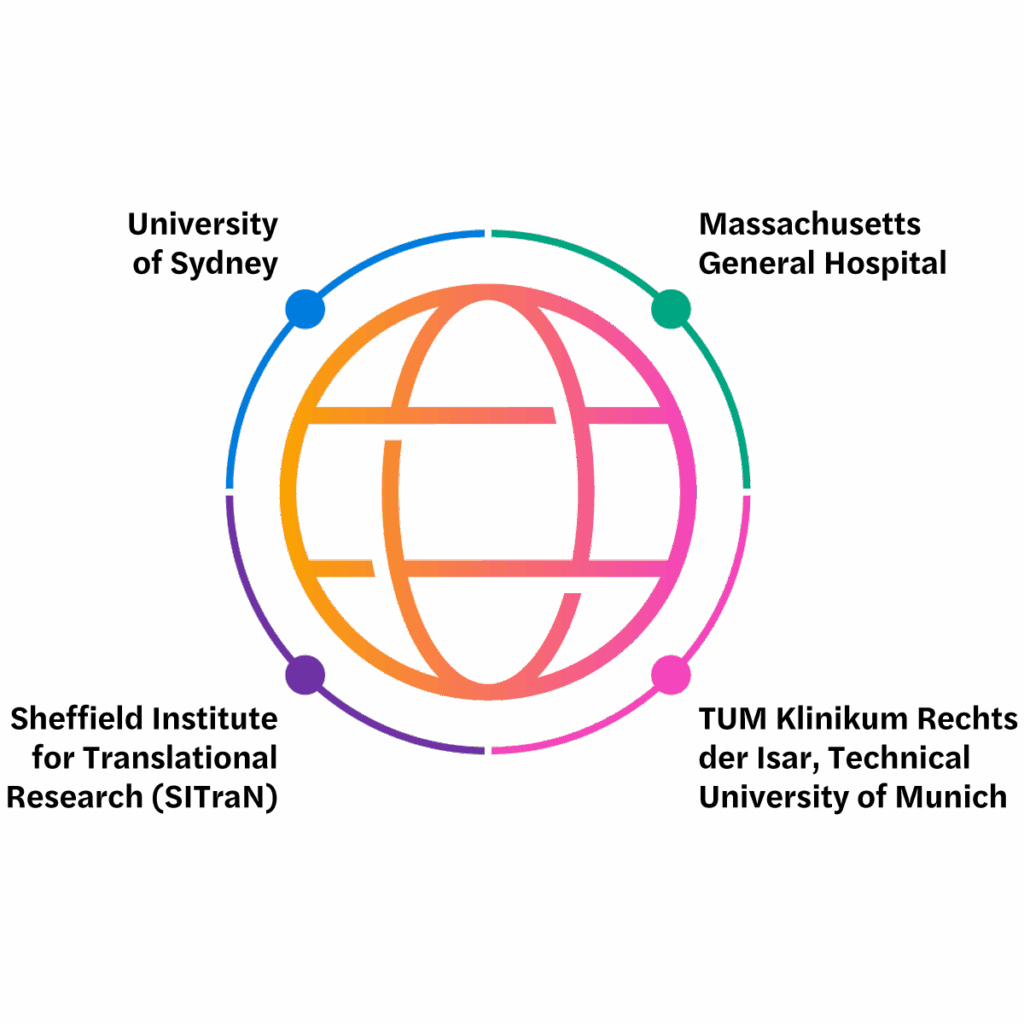
Our funded researchers will work together as an international research network to share best practices and collaborate to overcome barriers to developing repurposed drugs in MND.

To identify the best possible treatments for MND, we must cast a wide net – testing new hypotheses while ensuring we take advantage of previously developed therapies that could be re-tasked from unexpected sources.”
Adam Walker, University of Sydney, programme recipient
Challenges for MND drug repurposing
Knowledge gaps
Decisions to repurpose drugs are often based on insights from their original use, with limited understanding of how the drug works in the new disease area.
Projects will address gaps and increase confidence in drug selection for clinical trials.
Preclinical models
Promising results in preclinical models often fail to translate into meaningful clinical benefits for people with MND.
Projects will prioritise replication of drug data across multiple preclinical models, to better predict clinical benefits.
Combination approaches
Robust combination approaches are needed for drug screening and validation in preclinical and clinical research.
Projects will assess drug combinations to monitor drug interactions and effects.
Biomarkers
Clinical trials in MND need biomarkers to rapidly assess a drug’s efficacy.
Projects will identify and validate biomarkers for use alongside current approaches.
Target engagement
Evaluation of exposure and response to a drug remains essential for the development of repurposed drugs.
Projects need to demonstrate evidence that the repurposed drug reaches the target tissue, bind to its target, and produces the desired drug effect.
Commercial and logistical
LifeArc translational know-how will be made available to overcome some of the commercial and logistical challenges associated with repurposing both generic and on-patent drugs.
Repurposing projects we’ve funded through this programme
Validation of a drug target identified through multiomics
Led by Paul Lingor, TUM Klinikum Rechts der Isar, Technical University of Munich

Impaired nucleocytoplasmic transport has emerged as an important driver of disease in MND. Targeting this pathway with a drug currently in clinical use for other disorders, has been shown to protect neurons in preliminary studies using different models of MND.
This project will assess if this drug could work in MND by targeting several disease mechanisms at once.
Drug safety and long-term tolerability will be carefully considered in the potential success of this drug. Despite the potential for side effects, people living with MND and clinical experts were positive about its potential for repurposing in MND.
Collaborators include: a consortium of investigators from the Technical University of Munich (TUM); Ulm University, Germany; and Mario Negri Institute for Pharmacological Research, Italy.
Potential impact: If successful, this project will generate robust preclinical data on the treatment for MND, such as its ability to modulate disease progression and enhance survival of neurons.
Based on these findings, the team will develop a state-of-the-art clinical trial protocol for regulatory submission to advance this drug towards clinical testing in MND patients.
Jakinibs as potential repurposing candidates
Led by Richard Mead, University of Sheffield

MND is a complex disorder with multiple underlying disease-causing processes. Therapeutic treatments likely need to target different processes simultaneously across coexisting cells.
The team at Sheffield Institute for Translational Research (SITraN), used data science approaches to identify key disease mechanisms involved in MND. They proposed the JAK/STAT3 signalling pathway as a promising repurposing approach for MND. This pathway is targeted by a class of drugs called JAK inhibitors.
JAK/STAT3 signalling dysregulation has been implicated as a driver of MND through several mechanisms. The hope is that JAK inhibitors may simultaneously correct these interdependent processes to protect motor neurons.
The team is proposing a 2-year project to address current knowledge gaps for this class of drug.
Building on promising preliminary findings, they will assess how JAK inhibitors affect both peripheral and central MND disease mechanisms and undertake pharmacokinetic modelling studies to calculate a safe and effective dose for future clinical studies.
There are already several approved JAK inhibitors that are used for other illnesses including rheumatoid arthritis and myelofibrosis, and an assessment of the JAK inhibitor Baricitinib for use in MND is currently ongoing in the USA.
However, there are still knowledge gaps around using this class of drugs for MND.
Potential impact: The study will strengthen confidence that JAK inhibition could be beneficial in MND and provide information on how to progress these drugs for future clinical trials.

Patient representative for this project, Dr Ian Richard Bellion
Dr Ian Richard Bellion is a chemist and engineer with a career spanning both academic research and industry. He studied chemistry before completing the graduateship of the Royal Society of Chemistry at Kingston Polytechnic. He went on to earn his PhD in Food Science at University of Leeds.
Following a postdoctoral appointment, Ian transitioned from academia to a long career in industry. For 24 years, he worked as an engineer for Agilent Technologies, a leading technology company specialising in laboratory instruments.
After being diagnosed with MND in 2018, he returned to work but stopped working in late 2024 due to the progression of the condition. Ian takes a keen interest in MND research, and is proud to serve as a patient representative on the Jakinibs project team.
Repurposing heart medication to treat MND
Led by Brian Wainger, Sean M. Healey and AMG Center for ALS at Massachusetts General Hospital

The team has performed small molecule screens in neurons derived from human induced pluripotent stem cells (iPSCs). These included the use of two disease-relevant stressors: (1) synthesized toxic dipeptide repeat proteins (DPRs) to mimic C9orf72-associated MND and (2) proteasome inhibition to induce TDP-43 pathology.
From each screen, the FDA-approved heart medication digoxin emerged as a potent toxicity suppressor. Notably, other studies on MND and other neurodegenerative disease have also identified digoxin and its target, the sodium-potassium ATPase, as potential disease modifiers.
Digoxin has been widely used in heart conditions, such as arrythmias and heart failure, and safe doses are well established.
The project aims to generate robust preclinical data to understand more about the potential use of digoxin in MND. These include:
- determining whether digoxin enters the central nervous system
- evaluating whether digoxin can rescue signs of MND in animal models
- establishing biomarkers of digoxin action for use in a Phase II MND clinical study
Potential impact: If successful, the teams’ studies could support investigation of a well-established heart medication in clinical trials for MND.
Repurposing a cancer treatment drug for MND
Led by Adam Walker, University of Sydney

Aggregation of the TDP-43 protein within neurons of the brain and spinal cord is thought to cause nerves to degenerate in MND and is the hallmark of over 97% of MND cases.
Normally, a biochemical process called ‘autophagy’ (meaning ‘self-eating’) cleans up those protein aggregates inside nerve cells, but in MND this protective process is insufficient, and the nerve cells are damaged.
This project is tackling this problem by testing if a cancer drug, already in human clinical trials, could help people with MND by clearing these aggregates. Repurposing this drug to stimulate this protective autophagy process – which is useful in cancer to prevent tumour growth – could also slow nerve cell degeneration in MND.
To date the team have generated strong preliminary data showing that the drug can penetrate the central nervous system in mouse models of MND, resulting in decreased signs of disease, improved motor performance and increased survival. The drug also successfully engages the autophagy pathway.
The team will now address additional gaps in preclinical evidence for the cancer drug in MND. This includes:
- establishing the optimal dosing route and frequency
- testing if the treatment is effective in mouse models after the onset of disease and symptoms
- assessing drug-target engagement in the brain
The team also plan to pre-register their in vivo study methodology and analysis plans to test their hypothesis in multiple disease models to ensure robust replication of data.
Developing the project plan with regulatory experts and involving people with lived experience of MND has been a key part of the design of this study, to understand the gaps in data for this drug and to enable its safe and effective use for people living with MND.
Potential impact: If successful, this 3-year project will generate a data package to hopefully engage industry partners and secure additional follow-on funding for clinical studies for people living with MND.
MND Drug Repurposing Research Network
The MND Drug Repurposing Research Network maximises the impact of our funding and support for projects.
Ecosystem
- bring together lead investigators and research teams to overcome challenges in MND drug repurposing and increase impact
- create opportunities for effective collaboration and networking across projects
Translational knowledge
- create and share research best practices from preclinical to clinical stages
- provide opportunities to upskill project teams with expert translational advice and support
Asset progression
- promote the adoption of high-quality repurposed drug development approaches for MND
- support projects to generate robust and reproducible drug data packages
- involve people with lived experience to input on projects
Patient involvement
Our MND Insights Group, formed of people with lived experience, evaluated lay summaries of shortlisted programme applicants.

A review of best practices in MND drug discovery
Applicants were asked to refer to this review, published alongside our funding call, which outlines principles for improving preclinical research and de-risking MND clinical trials.
Contact us
In submitting your personal data via this form, you consent to being contacted via the details provided so that your enquiry can be responded to. If you would like your data to be removed, please email info@lifearc.org.
Please see our Privacy Policy in relation to the personal data you submit to us through this page.
This site is protected by reCAPTCHA and the Google privacy policy and terms apply.