The world’s largest study of the genetics of severe COVID-19, that we have helped to fund, reveals fresh information about why some people are more likely to become seriously ill with COVID-19.
In the GenOMICC study, which involves more than 57,000 people, researchers have discovered 16 new gene changes linked with the risk of developing severe COVID-19, including some related to blood clotting, immune response and inflammation.
The study deepens our understanding of how COVID-19 can affect the body and paves the way for new tests and treatments to protect people from infection.
Early in the pandemic, LifeArc provided £5 million to support the GenOMICC study, which aimed to uncover vital new information to help select existing drugs to treat COVID-19, and identify people most at risk of developing life-threatening symptoms.
These latest findings were published today in Nature Genetics.
Searching for genetic variants
One of the biggest mysteries of COVID-19 is why responses to SARS-CoV-2 infection vary so much from person to person. Although most people experience mild or no symptoms, some will develop severe disease that needs to be treated in hospital. While environmental factors – such as age, sex and pre-existing health conditions – account for some the difference, alterations in a person’s DNA also play a role.
In May 2020, researchers from the GenOMICC consortium – a global collaboration studying genetics in critical illness – in partnership with Genomics England, launched the GenOMICC study to identify key genetic variants involved in determining COVID-19 severity.
The team sequenced the whole series of genes (the genome) of 7,491 patients with severe COVID-19 from 224 intensive care units (ICU) in the UK. They compared the sequences with 48,400 other people who had not had COVID-19, participants in the 100,000 Genomes Project, and a further 1,630 people who had only experienced mild symptoms.
This work allowed the team to create a precise map and identify variations in DNA that were linked to severe COVID19. They found differences in 16 genes in the ICU group when compared to the DNA of the other groups, and confirmed seven other gene variations were also involved, that they had discovered in earlier studies.
Biological insights
These findings reveal clues to how we might tackle the disease.
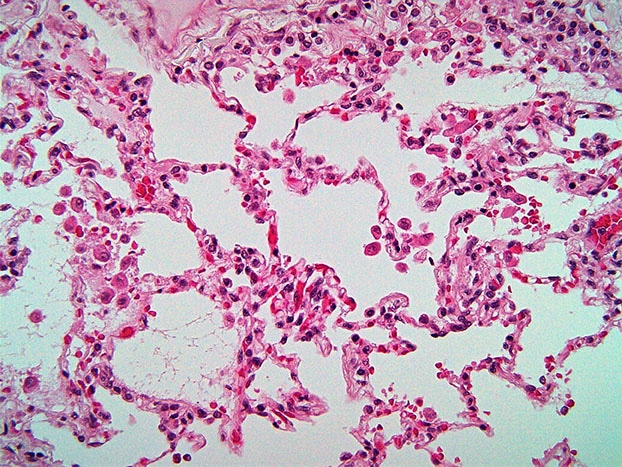
For example, the study a found a change in a single gene disrupts the amount of interferon alpha-10 produced by the body’s immune cells in response to an invading virus and increases a person’s risk of getting severe COVID-19. It suggests treating COVID-19 patients with interferons – drugs already used to treat different conditions involving the immune system – could help manage the disease.
This study also found gene variations controlling the levels of Factor VIII, a blood-clotting protein, were also a risk factor for severe COVID-19. This may help explain some of the clotting abnormalities seen in patients with life-threatening symptoms.
Professor Kenneth Baillie, who led the study at the University of Edinburgh, said: “Our latest findings point to specific molecular targets in critical COVID-19. These results explain why some people develop life-threatening COVID-19, while others get no symptoms at all. But more importantly, this gives us a deep understanding of the process of disease and is a big step forward in finding more effective treatments.
“It is now true to say that we understand the mechanisms of COVID-19 better than the other syndromes we treat in intensive care in normal times – sepsis, flu, and other forms of critical illness,” he continues. “COVID-19 is showing us the way to tackle those problems in the future.”
Identifying potential new treatments
Nearly two years into the pandemic, COVID-19 is continuing to cause thousands of deaths around the world each day and put healthcare systems under immense strain. There is still an urgent need to find new treatments for people who remain unvaccinated, whose immune systems do not fully respond to vaccination, or who experience breakthrough infections.
Dr Dave Powell, LifeArc’s Chief Scientific Officer said: “We’re delighted to have supported this exciting study that reveals more about the genetic profile of people who get critically ill with COVID-19.”
“These studies are important because they not only reveal important genetic factors that drive severe disease, but they could also highlight potential future treatment options for COVID-19, either through new drugs or existing drugs that could be repurposed,” he continued. “We are proud to be supporting the programme by helping the team decide which drugs to investigate and take forward.
“We’ll watch with interest as these discoveries advance the therapeutic pipeline towards the clinic, where they could ultimately help patients.”
LifeArc’s wider funding for COVID-19
Our funding for the GenOMICC study forms part of more than £27 million we have provided to support the search for new medicines and diagnostics to fight COVID-19, as well as mobilising our materials and our people to help the scientific community to tackle the pandemic.
Find out more about the other COVID-19 projects LifeArc has funded.